Healthcare / Population health
European Healthcare Design 2018
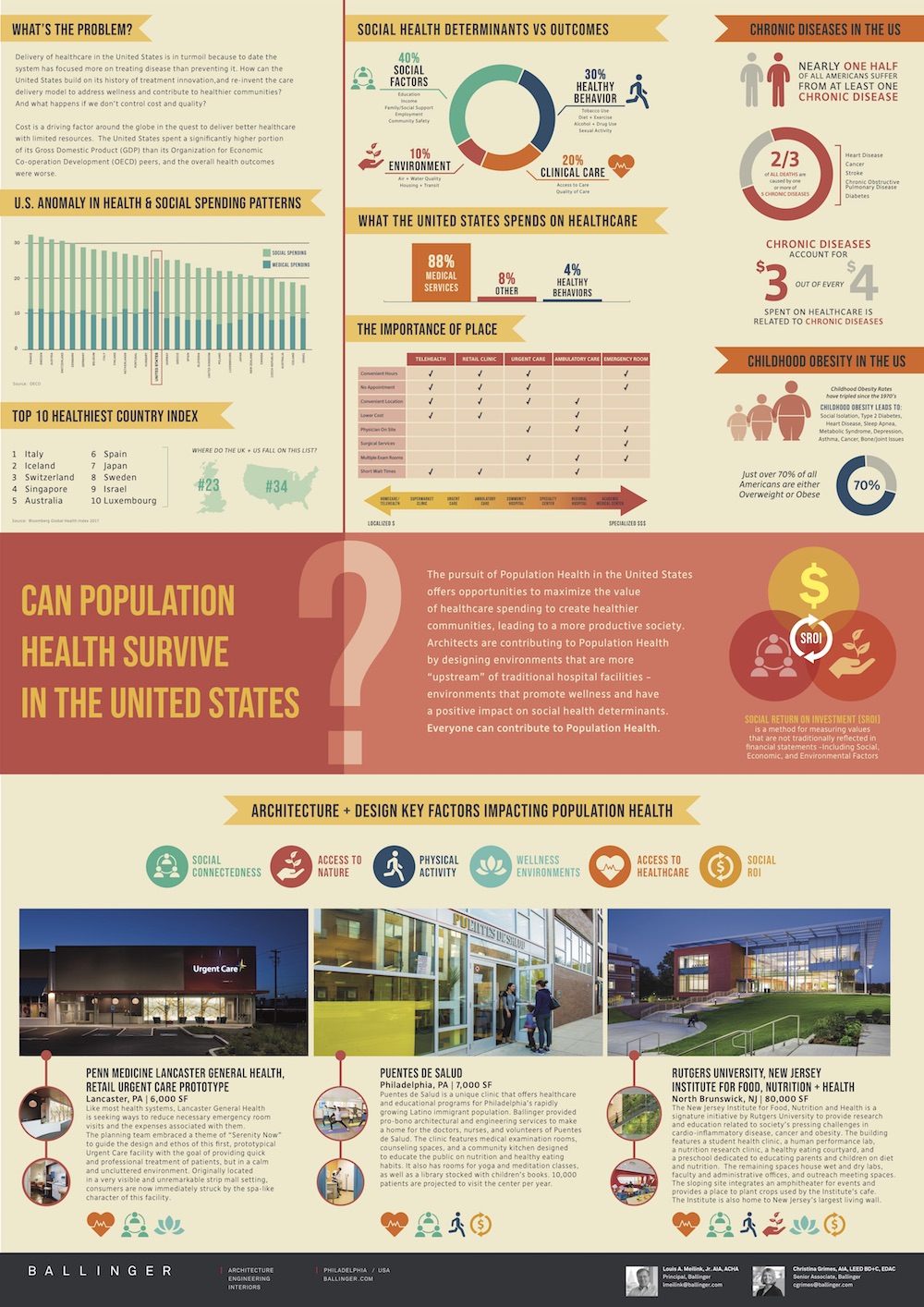
Can population health survive in the United States?
By Louis Meilink, Jr., AIA, ACHA, ACHE and Christina Grimes | 08 Jun 2018 | 0
This poster presentation will review the complex relationships between cause and effect in healthcare and how, as architects, we can design healthier environments that support an institution’s clinical goals and contribute to improving health in the larger community.
Abstract
Can population health survive in the United States?
Delivery of healthcare in the United States is in turmoil because, to date, the system has focused more on treating disease than preventing it. How can the United States build on its history of treatment innovation, and re-invent the care delivery model to address wellness and contribute to healthier communities? And what happens if we don’t control cost and quality?
Cost is a driving factor around the globe in the quest to deliver better healthcare with limited resources. The United States spent a significantly higher portion of its gross domestic product (GDP) than its peers from the Organization for Economic Co-operation Development (OECD), and the overall health outcomes were worse.
A 0.1-per-cent change in behaviour can result in a saving of US$2.7 billion in the United States alone. Each instance of bad behaviour and non-compliance contributes to sicker communities and rising costs. According to the Advisory Board, lack of transportation to see a health provider accounts for US$41,500 per patient per year as a single unaddressed barrier to care.
Purpose/objectives: This poster presentation will review the complex relationships between cause and effect in healthcare and how, as architects, we can design healthier environments that support an institution’s clinical goals and contribute to improving health in the larger community. The purpose of the presentation is to define how healthcare architects can help institutions navigate from the Triple Aim (the right care, at the right time, at the right cost) to a Quadruple Aim – care in the right place to increase access, and encourage better behaviour and compliance.
Methods and results: Beyond the hospital environment, thoughtful empathetic design can improve the spaces we inhabit on a daily basis and nudge better personal behaviours. Examples of how the design of buildings can contribute to improving health will be provided through specific case studies from George Washington University (Washington, DC), Lancaster Health Cancer Center (Pennsylvania, USA), and Reading Hospital (Pennsylvania, USA).
Conclusions: Through design, architects can alter the way communities conceptualise the notion of a hospital building and contribute to healthier lifestyles to control skyrocketing costs in a myriad of other ways. This new paradigm of population health offers opportunities to reduce the GDP percentage spent on healthcare and create healthier communities, all with the goal of a more productive society.
Organisations involved